Nursing practice is based on a foundation of information that is viewed, organized, and utilized in accordance with professional and personal influences. A nurse’s knowledge base includes theories, models, frameworks, and a philosophy of nursing. Personal influences impact both the client and nurse and include such components as values, health beliefs, stress, and the ability to respond to stress.
A. Evidenced-based practice
- Evidenced-based practice is the use of research to prove the efficacy of a specific action. Evidenced-based practice in the context of nursing is the performance of nursing interventions based on rigorous scientific evidence and clinical effectiveness studies rather than tradition, intuition, or anecdotal information.
- Research collects data that identifies which interventions will most likely produce expected client outcomes.
- Nursing practice based on evidence improves the quality of client care, justifies nursing interventions, expands the foundation of nursing as a profession, and may contain health-care costs.
B. Theory
- A theory is an organized set of ideas and concepts that assists one to find meaning in experiences, organize thinking around a concept or idea, and develop new insight.
- Way of viewing, describing, predicting, and controlling phenomena.
C. Model
- A model is a symbolic representation of a concept or framework.
- Can be described in words or an illustration.
D. Framework
- A framework is a broad, philosophical approach to a concept or idea.
- Usually presented in an outline format.
E. Value
- A value is something (e.g., quality, practice, or behavior) that a person holds in high regard.
- Influenced by family, religion, school, culture, and governmental traditions.
- Influences the formation of beliefs and attitudes.
F. Health belief
- A health belief is a concept about health that a person considers or accepts as accurate.
- Influenced by social, cultural, and spiritual values.
G. Philosophy
- A philosophy is a culturally determined system of beliefs, concepts, theories, or convictions.
- Influences one’s health practices (e.g., Jehovah’s Witnesses do not accept blood transfusions, and Catholics do not accept abortion).
II. NURSING THEORIES
Nursing theories identify and describe interrelated concepts that influence the practice of nursing. They provide a knowledge base that is broadly applicable to the variety of situations confronted by nurses. Each theory is unique, but they all include the client as the focus of the theory.
A. Self-care deficit theory of nursing—Dorothea Orem
1. Self-care is a purposeful learned behavior in response to a need.
2. Four concepts.
- Self-care: Self-initiated activities that a person performs to maintain life, health, and well-being.
- Self-care agency: An individual’s ability to engage in self-care based on developmental level, experiences, and available resources.
- Therapeutic self-care demand: Comprehensive self-care actions required to meet personal self-care requisites.
- Self-care requisites: Actions directed to meeting universal needs common to all people, such as air, water, food, elimination, activity, rest, solitude/social interactions, safety, and promotion of human function.
3. Nursing implications.
- Promotes nursing care, such as acting, doing for, guiding, teaching, supporting, and providing a supportive milieu that increases clients’ self-care abilities.
- Increases clients’ self-care activities to maintain life, health, and well-being.
B. Cultural care diversity and universality theory— Madeleine Leininger
1. Transcultural care is a central and uniting feature of nursing.
2. Focuses on cultural care that addresses:
- Preservation: Activities that help a client maintain health.
- Accommodation: Activities that promote ways a client adapts to and negotiates adjustments to health.
- Repatterning: Activities that help a client reconstruct life patterns to promote health.
3. Nursing implications.
- Requires nurses to view nursing as a transcultural care profession.
- Requires nurses to provide culture-specific care that assists clients to achieve and maintain health.
C. Human caring theory—Jean Watson
1. Care should be based on values of concern, kindness, love of self and others, and respect for the spiritual domain.
2. Explains that nursing is an interpersonal process.
3. Ten factors: The first three factors relate to the science of caring, and the rest relate to a focus of nursing practice.
- Forming values.
- Instilling faith and hope.
- Cultivating sensitivity to self and others.
- Developing a helping-trusting relationship.
- Promoting and accepting expression of positive and negative feelings.
- Using problem-solving for caring processes.
- Promoting transpersonal teaching and learning.
- Providing supportive, protective, or corrective mental, physical, sociocultural, and spiritual environments.
- Assisting with meeting needs while preserving dignity and wholeness.
- Being open to dimensions of caring and healing that cannot be scientifically explained.
4. Nursing implications.
- Supports caring as the basis of all nursing interventions and differentiates nursing from medicine, which is more concerned with curing.
- Encourages nurses to treat clients with care, respect, and dignity so that clients feel accepted, supported, and protected.
D. Adaptation model—Sister Callista Roy
1. A biopsychosocial adaptive system.
2. Involves a feedback cycle of input and output of stimuli.
3. Pronounces that a person modifies and integrates human and environmental components to achieve adaptation that supports survival, continuity, and growth.
4. States that people respond in four modes.
- Physiological-physical: Relates to basic physiological issues (e.g., oxygenation, exercise, nutrition, elimination, fluid and electrolyte balance, and temperature regulation).
- Self-concept: Relates to the physical self (e.g., threats to bodily functions) or personal self (e.g., anxiety, guilt, and distress responses to physical or emotional stressors).
- Role function: Relates to a client’s ability to adapt to physical and emotional stressors to maintain personal life roles.
- Interdependence Relates to issues that interrupt a client’s ability to maintain significant relationships.
5. Nursing implications.
- Promotes client adaptations in each of the four modes.
- Supports teaching about ways to alter internal and external environments to facilitate adaptations.
- Supports specific nursing care when adaptations are ineffective.
E. Functional health patterns—Marjory Gordon
1. Framework for organizing data.
2. Eleven health patterns.
- Health perception-health management.
- Nutritional-metabolic.
- Elimination.
- Activity-exercise.
- Sleep-rest.
- Cognitive-perceptual.
- Self-perception.
- Role-relationship.
- Sexuality-reproductive.
- Coping-stress tolerance.
- Value-belief.
3. Nursing implications.
- Facilitates the collection and organization of data.
- Promotes identification of interrelated information that assists nurses to determine clients’ health needs and appropriate nursing care.
F. Science of unitary human beings—Martha Rogers
1. Abstract theory focusing on a person as a cohesive whole with a dynamic energy field that constantly interacts with environmental energy fields.
2. Fields are characterized by a pattern, universe of open systems, and dimensionality.
3. Nursing implications.
- Encourages nurses to focus on a person’s wholeness.
- Promotes interventions based on interaction between human and environmental energy fields, such as therapeutic touch and direct/ redirect patterns of interaction to increase achievement of health.
- Attempts to maintain an environment free from negative energy.
III. Theoretical Foundations Related to Concepts of Health, Wellness, and Illness
Health, wellness, and illness are terms used by people to reflect how they feel physically and/or emotionally. These terms, although used universally, are highly individualized, subjective, and influenced by a variety of factors. Theories have been developed to facilitate an understanding of the concepts and relationships between health, wellness, and illness.
A. Definitions of health
1. Is highly personal and subjective and is based on one’s individual perception.
2. “A state of complete physical, mental, and social well-being and not merely the absence of disease or infirmity,” according to the World Health Organization (1948).
3. “A dynamic state of being in which the developmental and behavioral potential of an individual is realized to the fullest extent possible,” according to the American Nurses Association (1980).
4. “An experience that is often expressed in terms of wellness and illness and may occur in the presence or absence of disease or injury,” according to the American Nurses Association (2004).
B. Definition of wellness
“A way of life oriented toward optimal health and well-being in which body, mind, and spirit are integrated by the individual to live more fully within the human and natural community,” according to Myers, Sweeney, and Witmer (2000).
C. Definition of illness
1. A state in which a person’s status (e.g., physical, emotional, spiritual, developmental, intellectual, social) is diminished or impaired.
2. Not a disease but rather a response to a disease.
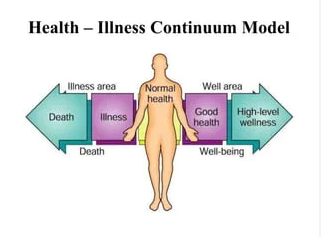
D. Health-illness continuum
1. The health-illness continuum is viewed along a continuum, with no distinct boundaries, that ranges from an excellent level of health to serious illness.
2. Placement on the continuum is determined by a person’s self-perception and the perceptions of others; perceptions are influenced by many factors.
3. Placement on the continuum is dynamic and may change at any time.
4. Nursing implications.
- Requires nurses to explore their own perceptions about health and illness and not impose them on clients.
- Assists nurses to identify where clients place themselves on the health-illness continuum because clients’ health beliefs influence nursing care.
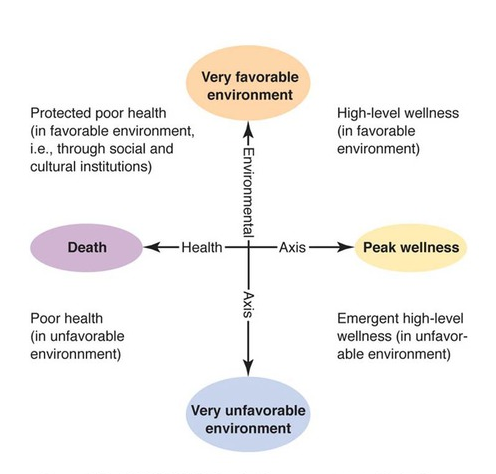
E. High-level wellness grid—H. L. Dunn
1. Allows a client’s status to be plotted along an axis from peak wellness to death and against an intersecting axis from a very favorable environment to a very unfavorable environment.
2. Based on the intersection of the two axes, four quadrants of health and wellness are formed.
- Protected poor health(in favorable environment).
- Poor health(in unfavorable environment).
- High-level wellness(in favorable environment).
- Emergent high-level wellness(in unfavorable environment).
3. Examples of environments.
- Favorable: Health insurance to pay for health services; supportive, caring family members; clean, uncrowded home environment.
- Unfavorable: Indigence or poverty; role responsibilities that interfere with health-seeking behaviors; lack of family; dirty, crowded home environment.
4. Nursing implications.
- Allows nurses to identify environmental factors that influence a client’s level of wellness.
- Facilitates prediction of whether clients’ health will likely improve or decline on the basis of support or lack of support within the environment.
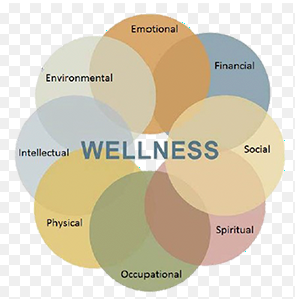
F. Wellness model—Anspaugh, Hamrick, and Rosato
1. To achieve health and wellness, a client must deal with features and dynamics within each of seven components of wellness.
- Physical.
- Social.
- Emotional.
- Intellectual.
- Spiritual.
- Occupational.
- Environmental.
2. Wellness requires working on all components of the model.
3. Nursing implications.
- Requires nurses to assess clients from seven perspectives.
- Facilitates a holistic approach to caring for clients because all components of wellness must be addressed.
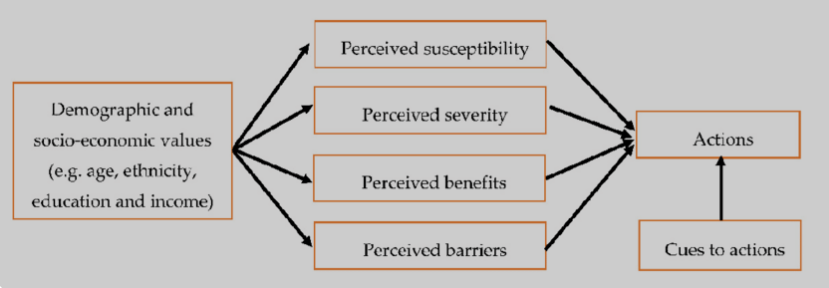
G. Health belief model—Becker, Maiman, and Rosenstock
1. Addresses the relationship between an individual’s beliefs and behaviors.
2. Three components.
- Individual’s perception of susceptibility to illness.
- Individual’s perception of the seriousness of the illness.
- Individual’s potential for action, which depends on benefits and barriers to taking action.
3. Nursing implications.
- Facilitates an understanding of client behaviors.
- Provides a prediction of how clients might behave.
- Provides a basis for client teaching.
H. Role performance model
1. Recognizes that all people generally fulfill a number of societal roles, such as parent, daughter or son, friend, and employee.
2. People who are able to fulfill their roles are considered healthy even though they may have an illness or disability.
3. Implies that people are unhealthy if they are unable to fulfill their roles.
4. Nursing implications.
- Requires nurses to explore client perceptions about role performance versus the sick role to help plan and implement nursing care.
- Obligates nurses to foster independence when caring for clients who define their level of health by their ability to provide self-care.
I. Clinical or medical model
1. Interpretation of health is based on the presence or absence of signs and symptoms of illness, disease, or injury; a narrow interpretation of health.
2. A person is considered either healthy or sick; there is no continuum.
3. The model is based on the perception that a person is a physiological system with associated functions.
4. Nursing implications.
- Focuses on making nursing assessments in the physiological realm.
- Requires nurses to explore domains other than the physiological realm because this theory has a narrow interpretation of health.
IV. Theoretical Foundations of Nursing Practice
Nursing practice is an art and science that bases nursing care on information from a variety of disciplines (e.g., physical, social, and natural sciences) and related conceptual frameworks. A conceptual framework presents related ideas, statements, and concepts that address their significant interrelationships, providing an organized perspective to complex situations and problems. Theories that influence the discipline of nursing include those that present a framework reflective of growth and development, psychosocial issues, human needs, and grief and loss.
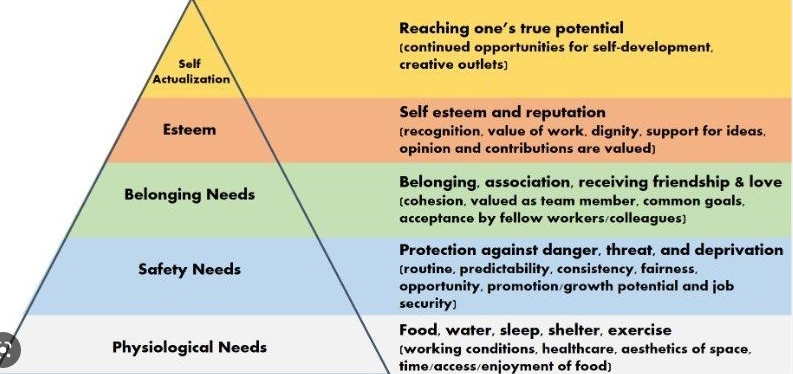
A. Hierarchy of basic human needs model—Abraham Maslow
1. Human needs are arranged in a hierarchy of importance.
a. Physiological: Includes basic needs essential to maintain life (e.g., air, water, food, elimination, rest, sleep, sex, and activity).
b. Safety and security: Includes the need to be physically and emotionally protected from injury (e.g., performing hand hygiene, sterile technique, effective mobility, and activities that promote trust; ensuring that the call bell is within the client’s reach, wheels are locked on equipment, and the bed is maintained in the lowest position; and explaining care before initiation).
c. Love and belonging: Includes the need to give and receive love and acceptance and have a significant connection to family members, friends, and the community (e.g., treating clients with respect, ensuring privacy, and involving family members in care when appropriate).
d. Self-esteem: Includes the need to have a positive self-regard, feel appreciated, and be independent and confident (e.g., encouraging independence, facilitating attainment of realistic goals, supporting roles, and accepting clients’ values and beliefs).
e. Self-actualization: Includes the need to achieve the highest potential within abilities (e.g., accepting clients as unique individuals, focusing on strengths, supporting hope, and teaching clients to be proactive in reaching their own potential).
2. Human needs motivate behavior.
3. Lower-level needs must be met to some degree before higher-levels needs are met.
B. Theory of psychosocial development—Erik Erikson
1. Based on interrelationships between emotional and physical variables rather than psychosexual stages.
2. Individuals at various stages of development cope with conflicts that may have a favorable or unfavorable outcome.
3. Extent of resolution of preceding stage influences subsequent stages.
4. Nursing implications.
- Helps nurses understand human behavior.
- Helps nurses identify clients’ stages of development and extent of task achievement.
- Helps nurses assist clients to develop coping skills associated with each task.
C. Theory of cognitive development—Jean Piaget
1. Thinking and reasoning develop through exposure to new experiences.
2. Four phases.
- Sensorimotor: Birth to 24 months; characterized by cognition, primarily through the senses and ability to process information on the physiological or emotional level.
- Preoperational: 2 to 7 years of age; characterized by an increasing ability to connect cognitively through language and actions.
- Concrete operations: 7 to 11 years of age; characterized by an increasing ability to organize information and use logical thought, ability to solve concrete problems, and less egocentricity.
- Formal operations: 11 to 15 years of age; characterized by use of abstract thinking and deductive reasoning and ability to examine alternatives.
3. Movement through phases is based on inherited intellect and environmental impact.
4. Each phase developed through:
- Adaptation: Ability to adjust to and interact with the environment.
- Assimilation: Inclusion of new experiences and information within one’s knowledge.
- Accommodation: Change in one’s knowledge as a result of processing new experiences and information.
5. Nursing implications.
- Allows nurses to design nursing care, teaching plans, and activities that are appropriate for a child’s developmental level.
- Helps nurses identify a child’s developmental level and determine how far ahead to prepare the child for a procedure.
D. Developmental stages and tasks—Robert Havighurst
1. Each stage has a task requiring mastery.
2. Mastery of preceding tasks is essential for mastery of future tasks.
3. Six stages.
- Infancy and early childhood: Birth to 6 years of age.
- Middle childhood: 6 to 13 years of age.
- Adolescence: 13 to 18 years of age.
- Early adulthood: 19 to 30 years of age.
- Middle adulthood: 30 to 60 years of age.
- Later maturity: 60 years of age and older.
4. Nursing implications.
- Provides guidelines for supporting and evaluating task achievement.
- Facilitates identification of lack of task achievement, which requires interventions.
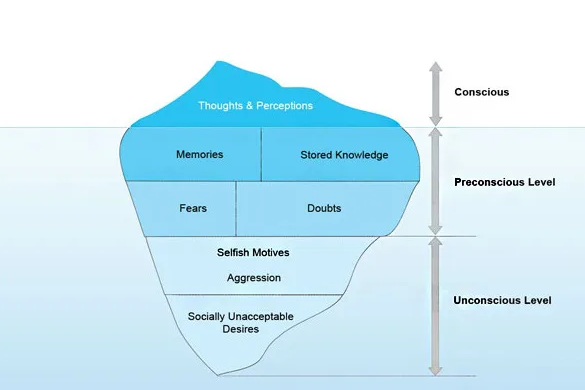
E. Psychoanalytic theory—Sigmund Freud
1. Childhood experiences form unconscious motivation for behavior.
2. The basis of the theory is the development of balance between pleasure-seeking instincts and the standards of society.
3. Sexual energy is centered in body parts at different ages.
- Oral: Birth to 12–18 months.
- Anal:12–18 months to 3 years.
- Phallic or oedipal:3 to 6 years.
- Latency:6 to 12 years.
- Genital: Puberty through adulthood.
4. The personality has three parts.
- Id (sexual energy): Represents instinctual urges, pleasures, and gratification; dominant in infants and children.
- Ego(realistic part of self): Balances what is wanted (demands of the id) and what is possible in light of societal limitations; begins to develop at 4 to 6 months of age.
- Superego(conscience): Regulates and restrains behavior by balancing the demands of the id and pressures of society; begins to develop at 5 to 6 years of age.
5. Nursing implications.
- Helps nurses to understand human behavior.
- Allows nurses to develop a plan of care based on a client’s psychosexual development and personality needs.
F. Theory of stages of moral development—Lawrence Kohlberg
1. Theory helps to explain the development of moral code.
2. Each stage builds on the previous stage and develops over time.
3. Based on the ability to think at a higher level as one matures.
4. Based on the study of boys; validity of application to females is criticized.
5. Six stages.
- Obedience and punishment: Motivation for behavior is fear of negative consequences (e.g., punishment, disapproval).
- Individualism and exchange: Motivation for behavior is the desire for a positive consequence (e.g., good result, reward).
- Interpersonal relationships: Motivation for behavior is based on pleasing others because it is what others expect.
- Maintaining social order: Motivation for behavior is based on following rules.
- Social contract and individual rights: Motivation for behavior is based on differing values, beliefs, and opinions but adheres to standards agreed upon by society.
- Universal principles: Motivation for behavior is based on abstract reasoning, universal ethical principles (e.g., the “Golden Rule”), and principles of justice.
6. Nursing implications.
- Increases nurses’ understanding that client decision making is influenced by one’s moral code.
- Helps nurses examine their own moral code and not impose their moral orientation onto clients and their family members.
G. Faith development—James Fowler
Faith represents a set of beliefs and values that develop over time as a person ages. According to the faith development theory by James Fowler (1981), an individual progresses through six stages adding new patterns of values, beliefs, and ways of thinking as one ages from a preschooler to adulthood.
V. The Profession of Nursing
Nursing is considered both a profession and a discipline. As a profession, it is based on technical and scientific knowledge; has members who are knowledgeable, competent, and evaluated by peers; and has a code of ethics. As a discipline, nursing has its own scientifically based body of knowledge involving both a theoretical foundation and a practical aspect in the form of clinical skills. In addition, nursing integrates knowledge and principles associated with other disciplines, such as anatomy and physiology, psychology, sociology, communication, and mathematics. A variety of nursing education programs, from those providing entry into practice through the doctoral level, prepare nurses to practice as professional nurses on various levels of nursing practice and in various health-care settings. Nursing organizations support the practice of nursing by activities such as publishing position statements on important issues affecting nursing, encouraging and supporting nursing scholarship and research, and identifying standards of nursing practice and codes directing nursing practice. In addition, they recognize expertise via certification of professional nurses who demonstrate proficiency in a specific area of nursing practice. Nurses should understand the educational programs available to continue personal growth and the ser vices that nursing organizations provide to the profession of nursing.
A. Definitions of nursing
1. According to the International Council of Nurses (ICN) (2002), which represents nurses throughout the world, “Nursing encompasses autonomous and collaborative care of individuals of all ages, families, groups and communities, sick or well and in all settings. Nursing includes the promotion of health, prevention of illness, and the care of ill, disabled and dying people. Advocacy, promotion of a safe environment, research, participation in shaping health policy and inpatient and health systems management, and education are also key nursing roles.”
2. According to the American Nurses Association (ANA), which represents nurses throughout the United States, “The protection, promotion, and optimization of health and abilities, prevention of illness and injury, alleviation of suffering through the diagnosis and treatment of human response, and advocacy in the care of individuals, families, communities, and populations” (2016).
B. Nursing organizations
1. American Nurses Association (ANA).
- Mission: “Nurses advancing our profession to improve health for all.”
- National professional organization for nursing in the United States.
- Involved in such activities as publishing standards of nursing practice; lobbying for professional, political, and economic issues impacting health care and nursing; and certifying expert nurses who meet experiential and testing criteria.
- Online at www.nursingworld.org.
2. National League for Nursing (NLN).
- Mission: “Promote excellence in nursing education to build a strong and diverse nursing workforce to advance the health of our nation and the global community.”
- Organization of individuals such as nurses, non-nurses, and agencies.
- Involved in such activities as providing a voice for nursing education and advocates for nurse educator interests in academic, professional, and political arenas.
- Online at www.nln.org.
3. National League for Nursing Accrediting Commission (NLNAC).
- Mission: “Supports the interests of nursing education, nursing practice, and the public by the functions of accreditation.”
- Involved in such activities as accrediting nursing education programs, both postsecondary and higher degree, that offer either a certificate, diploma, or recognized professional degree.
- Online at www.nlnac.org.
4. International Council of Nurses (ICN).
- Mission: “To represent nursing worldwide, advancing the profession and influencing health policy.”
- Involved in such activities as representing the profession of nursing worldwide via a federation of national nursing associations and collaborating with other organizations to provide access to focused information and research on major nursing and health topics (e.g., International Center for Nursing Human Resources).
- Online at www.icn.ch.
5. National Student Nurses’ Association (NSNA).
- Mission: “To mentor students preparing for initial licensure as registered nurses, and to convey the standards, ethics, and skills that students will need as responsible and accountable leaders and members of the profession.”
- Involved in such activities as representing student nurses; convening yearly conventions; and publishing Image,the official journal of the NSNA.
- Online at http://www.nsna.org.
6. Sigma Theta Tau International (STTI), the honor society of nursing.
- Mission: “Advancing world health and celebrating nursing excellence in scholarship, leadership, and service.”
- Selects students in baccalaureate, masters, doctoral, and postdoctoral programs and practicing nurses for membership when they demonstrate excellence in nursing.
- Has a scholarly purpose rather than a social purpose.
- Involved in such activities as providing awards and grants supporting nursing research; conducting biennial conventions to address organizational business and programs; and supporting a leadership institute, nursing research library, and global initiatives.
- Online at www.nursingsociety.org.
C. Nursing education
1. Programs that prepare students to take the National Council Licensure Examination for Registered Nurses (NCLEX-RN).
a. Diploma programs. (1) Were the most common nursing programs before the 1960s, when nursing education moved into community college and university settings; have dramatically declined in number. (2) Generally are under the sponsorship of a hospital and may provide college credit if associated with a community college. (3) Generally take 3 years to complete and focus on clinical experience.
b. Associate degree programs, such as associate degree in nursing (ADN), associate of arts (AA), associate of science (AS), or associate in applied science (AAS). (1) Generally are 2-year programs offered by a community college or university; however, because many students are older with family and job responsibilities, may take 3 or more years of part-time study to complete. (2) Provide the basis for pursuing more advanced nursing education.
c. Baccalaureate degree nursing programs, such as bachelor of science in nursing (BSN). Offer two courses of study. (1) Generic: Generally are 3- to 4-year programs for students entering as freshmen with a major in nursing. (2) General: Generally are 2-year programs for graduates of ADN programs or diploma programs with college credit; may offer a “fast track” option (1 to 11⁄2 years of continuous classes).
d. Master’s entry program in nursing if the student earned a baccalaureate degree in another field.
e. Doctoral entry program in nursing, which is similar to master’s entry; has limited enrollment.
2. Licensed practical nurse or vocational nurse programs that prepare students to take the National Council Licensure Examination for Practical Nurses (NCLEX-PN).
a. Prepare graduates to provide uncomplicated bedside nursing care under the supervision of an RN.
b. Generally are 1 to 11⁄2 years in length.
3. Programs that provide advanced degrees in nursing.
a. Master’s degree nursing programs, such as master of arts (MA), master of science (MS), master of science in nursing (MSN), and master in nursing (MN). (1) Prepare RNs with a BSN degree for advance practice. (2) Prepare nurses to assume advanced roles in clinical practice, education, research, and administration, such as clinical nurse specialist (CNS), certified nurse midwife (CNM), certified registered nurse anesthetist (CRNA), nurse practitioner (NP), nurse administrator, and professor of nursing education. (3) Generally take 11⁄2 to 2 or more years to complete.
b. Doctoral programs in nursing, such as doctor of philosophy (PhD), doctor of nursing science (DNS, DNSc), and nursing doctorate (ND). (1) Prepare nurses with master’s degrees in nursing for advanced practice. (2) Focus of programs varies, such as clinical practice, administration, education, and theory development; however, all emphasize research.
D. Nursing certification
1. Nursing certification is documentation that recognizes and certifies the status, level of achievement, or expertise of a nurse in a specific area of nursing practice.
2. Achieved in areas of practice, such as geriatrics, medical-surgical nursing, pediatrics, emergency nursing, nursing administration, nursing education, community health nursing, school nursing, and maternal-child nursing.
3. Provided by the ANA or specialty nursing organizations.
E. Continuing education
1. Continuing education is instruction received after leaving a formal educational system, generally consisting of short or part-time courses.
2. Many states require a certain number of hours of ongoing education (e.g., 15 to 30 hours every 2 years) or completion of classes on a specific topic (e.g., infection control, child abuse) for RN licensure renewal.
3. Classes ensure that nurses keep abreast of new technology, theories, and clinical practice.
4. Programs are offered by employers, colleges, professional nursing organizations, and professional journals.
F. In-service education
1. In-service education is instructions or educational programs provided by employers.
2. Generally focus on new equipment, introduction of new policies or procedures, or topics mandated by a state health department, such as infection control and cardiopulmonary resuscitation.






