The ability to produce and eliminate waste in the form of urine is essential for life. The mechanisms of glomerular filtration and the production of urine are complex and require an integration of factors, involving effective functioning of the kidneys, ureters, urinary bladder, and urethra. In addition, elimination of urine in the male is influenced when an enlarged prostate gland causes obstruction of the urethra. Knowledge of anatomy and physiology that influences urinary elimination is the basis for understanding how to best care for clients with urinary elimination problems.
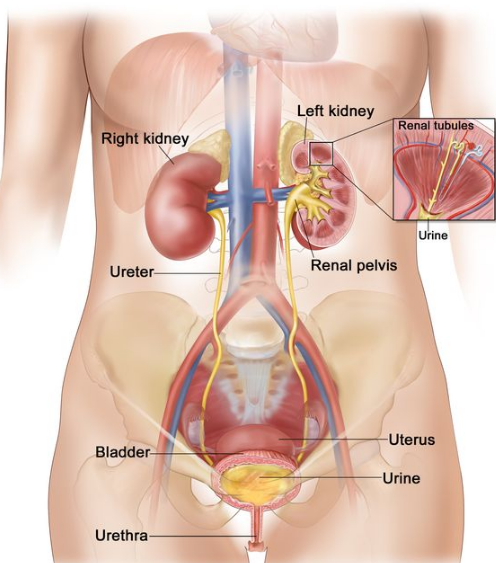
A. Kidneys
- Filter metabolic waste, excess ions, bacterial toxins, water-soluble drugs, drug metabolites, and water from the blood and excrete them as urine.
- Form urine by filtration, reabsorption, and secretion.
- Regulate blood volume, blood pressure (BP), fluid and electrolyte balance, and acid-base balance.
- Secrete rennin that causes the conversion of angiotensinogen to angiotensin I, which is subsequently converted to angiotensin II, which stimulates the nephrons to promote sodium and water retention.
- Secrete erythropoietin, which acts on the bone marrow to produce red blood cells.
- Converts part of calcidiol, a vitamin D metabolite, to calcitriol, the biologically active form of vitamin D, which travels in the blood to control the concentration of calcium and phosphate and promote growth and remodeling of bone.
- Produce a volume of filtrate in 1 minute (glomerular filtration rate [GFR]).
B. Ureters
- Transport urine produced by the kidneys to the bladder.
- Funnel shaped at the renal pelvis.
- Are 10 to 12 inches (25 to 30 cm) in length.
- Enter the bladder at the posterior corners of the bladder floor.
C. Bladder
- Receives urine from the ureters.
- Stores urine (600 to 1,000 mL) until it is eliminated.
- Urge to eliminate is stimulated by 200 to 250 mL of urine.
D. Urethra
- Transports urine from the bladder and semen from the prostate gland in males to outside the body.
- Is 1.5 to 2 inches long in a female and 8 inches in a male.
- Opens at the urinary meatus.
E. Prostate gland (male)
- Ring-like gland through which the urethra passes.
- Contracts rhythmically and secretes prostatic fluid with male ejaculate, which has an alkaline pH that helps sperm to survive in the acid environment of the female reproductive tract and mobilizes sperm after ejaculation
II. Urination
After urine is produced, it is stored in the bladder until voiding occurs. The ability to void requires an integrated operative functioning of the bladder, urethra, brain, spinal cord, and peripheral nerves supplying the bladder and urethra. In addition, a person must be able to recognize and respond to the urge to void. A nurse must understand the integrated operative function of urination and identify the expected characteristics of a client’s urine and common problems associated with the urinary system to better meet a client’s urinary elimination needs.
A. Process of urination
- Urination (voiding, micturition)is the act of emptying the urinary bladder.
- The detrusor muscle in the bladder contracts, urging stored urine through the relaxed internal urethral sphincter into the urethra, which results in a conscious urge to void.
- The external urethral sphincter inhibits the release of urine until a person is ready to urinate; once ready, the brain signals the external sphincter to relax and further detrusor muscle contraction empties the bladder.
B. Urine characteristics
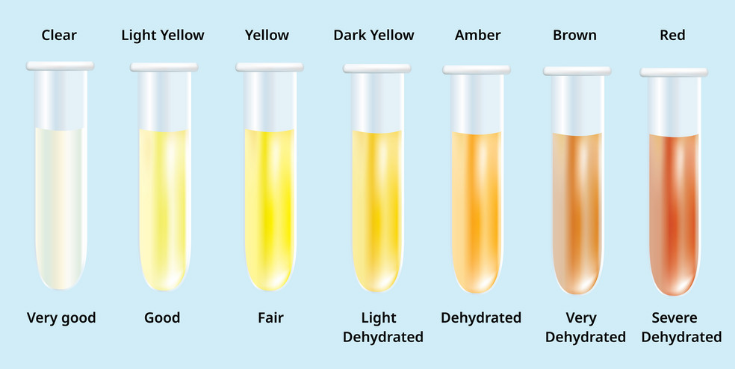
1. Color.
- Indicates the degree of concentration.
- Usually straw colored, pale to amber.
2. Clarity or turbidity.
- Usually transparent or translucent.
- Cloudiness indicates the presence of abnormal constituents.
3. Amount.
- Indicates the volume of production and excretion of urine.
- Usually 1,200 to 1,500 mL daily.
4. Odor.
- Is aromatic.
- Can indicate the presence of certain foods and constituents related to infection.
5. Specific gravity.
- Reflects the kidneys’ ability to concentrate urine.
- Usually 1.001 to 1.029.
6. pH.
- Reflects the kidneys’ ability to maintain a balanced hydrogen ion concentration in the blood.
- Usually between 4.6 and 8; average is 6.
7. Protein.
- Exists in molecules that generally are too large to leak into the glomerular filtrate, but leakage can occur in the presence of glomerular damage or impaired tubular reabsorption.
- A random urine specimen for protein more than 6 mg/dL when tested with a dipstick indicates renal disease.
- The amount of protein in a 24-hour specimen indicates the severity of kidney disease; an expected 24-hour result is 25 to 150 mg.
C. Abnormal characteristics of urine and their implications.
III. Factors Affecting Urinary Function
Age, psychosociocultural influences, nutrition, hydration, activity, position, mobility, medical problems, surgical and diagnostic procedures, ability to communicate, and medications can dramatically affect urinary function. Understanding these factors will aid nurses in assessing clients, maintaining a nonjudgmental attitude when working with diverse individuals, and planning individualized nursing care.
A. Developmental
1. Infants. a. Generally produce 8 to 10 wet diapers daily. b. Develop voluntary control at 18 to 24 months of age.
2. Children: May experience involuntary passage of urine when awake (enuresis)or when sleeping (nocturnal enuresis).
3. Older adults.
- Experience a decline in urinary system function.
- Are less able to filter waste and maintain acid base and fluid and electrolyte balance.
- Experience a loss of bladder tone, contributing to urgency, frequency, and incomplete emptying of the bladder.
- Older women: Experience additional weakening of pelvic floor muscles due to childbearing and genitourinary atrophy.
- Older men: May experience an enlarged prostate, causing urine leakage, awakening at night to void (nocturia),and urine retention.
B. Psychosociocultural
- Lack of privacy or an unfamiliar environment may lead to an inability to void in public (bashful bladder).
- Loss of dignity related to toileting activities in a health-care environment, especially if the client is catheterized, can cause emotional distress.
- Cultural influences may cause a person to insist on a caregiver of the same gender to provide toileting assistance.
- Muslims use the left hand for toileting activities and the right hand for eating and praying.
C. Nutrition and hydration
- As fluid intake increases, a corresponding increase in urine output occurs; as fluid intake decreases, a corresponding decrease in urine output occurs.
- Some substances increase urine production (e.g., coffee, tea, cola, alcohol, and chocolate) by inhibiting the release of antidiuretic hormone.
- Sodium intake produces water retention, causing decreased urine production.
D. Activity and position
- Exercise maintains detrusor and pelvic floor muscle tone, which helps the bladder to empty completely.
- Heavy exercise can precipitate dehydration via sweating, causing the kidneys to retain water, reducing urine output.
- Gravity assists in the flow of urine and the ability to empty the bladder completely; typically, the sitting position is best for women and the standing position is best for men.
- The bladder may not empty completely when on a bed pan or when using a urinal while lying flat; the side-lying position may facilitate urination for men who are on bedrest.
E. Medications and anesthetic agents
- Many classifications of drugs can damage kidney cells (nephrotoxic)or cause urinary retention, such as antispasmodics, antihistamines, tricyclic anti depressants, anticholinergics, antihypertensives, antiparkinsonism drugs, and chemotherapeutic agents for cancer.
- Diuretics cause an increase in urine production; if urine output is excessive in relation to fluid intake, dehydration occurs; urine output decreases when a client is dehydrated.
- Some drugs change the color of urine; for example, phenazopyridine causes the urine to appear reddish orange.
- Anesthetic agents generally decrease BP and GFR, causing a decrease in urine production; spinal anesthesia reduces the perception of the need to void, leading to bladder distention.
F. Physiological problems
- Problems can interfere with the production of urine; for example, cardiovascular and metabolic disorders that reduce blood flow through the kidneys (e.g., hypertension, heart failure, shock, and diabetes mellitus).
- Problems can impair the nervous system that innervates the urinary system; for example, brain attack (stroke) or spinal cord injury.
- Problems can interfere with the flow of urine; for example, calculi and enlargement of the prostate gland.
- Problems can cause inflammation of the structures of the urinary system; for example, urinary tract infection (UTI).
- Impaired cognition (e.g., delirium, dementia) or a mental health problem may alter a person’s perception of the need to void.
G. Surgical and diagnostic procedures
- Rectal, vaginal, and pubic surgery and childbirth can result in trauma to and edema of local tissues, causing pressure on the structures of the urinary system and loss of pelvic floor muscle control.
- Some surgical procedures (e.g., hysterectomy, transurethral resection of the prostate) require insertion of a temporary indwelling urinary catheter postoperatively.
- Insertion of a fiberoptic instrument (cystoscope) through the urethra to examine the bladder (cystoscopy)can cause urethral swelling, obstructing urinary excretion.
H. Communication or mobility problems
- An inability to communicate the need to void can result in what appears to others to be an episode of incontinence when in fact the client cannot indicate personal needs to others.
- An inability to engage in toileting activities, such as undressing, can result in episodes of urination before reaching a toilet.
- An inability to be mobile, such as with clients who are bed- or chair-bound, may prevent a client from obtaining assistance in time to make it to the bathroom.
IV. Assessment of the Urinary System
The first step of the nursing process is assessment. When collecting information relative to a client’s urinary function, the nurse obtains a client history, performs a physical assessment, and assesses the volume and characteristics of urine. Data collected from these assessments help determine whether the client’s urinary system is functioning adequately or further action is required by a nurse or the primary health-care provider.
A. Obtain a health history
1. Identify any change in urination habits or urine characteristics.
2. Ask questions about the presence of clinical manifestations that indicate infection.
- Urinary urgency is a strong desire to void.
- Urinary frequency is voiding that occurs more often than usual.
- Dysuria is painful or difficulty voiding.
- Hematuria is blood in the urine.
3. Ask questions about the clinical manifestations of urine flow.
- Urinary hesitancy is a delay in initiating voiding.
- Nocturia is the awakening at night to void.
- Overflow incontinence is the involuntary frequent passage of a small amount of urine in conjunction with a distended bladder.
- Urinary incontinence is the involuntary passage of urine.
4. Ask about daily urine volume.
- Oliguria is when urine output is less than 500 mL daily (oliguria).
- Polyuria is an abnormally large volume of urine output daily.
- Anuria is the absence of urine output or urine output of less than 100 mL daily.
5. Assess for flank pain that indicates a problem with the kidneys.
6. Identify a history of urinary system problems (e.g., infection, kidney or bladder problems, urinary tract surgery or urinary system diagnostic procedures or tests).
7. Assess lifestyle factors that can affect the urinary system (e.g., daily caffeine and fluid intake, smoking history, management of activities of daily living, emotional stress, and access to a bathroom).
8. Identify any medications the client is currently taking that may impact the urinary system.
9. Ask how long the client has been experiencing any identified problems; how the client manages the problem; and what has been done medically.
B. Perform a physical assessment
1. Assess the characteristics of urine.
2. Measure intake and output (I&O).
3. Assess for weight gain and edema.
4. Palpate the suprapubic area for bladder distention if the client is unable to void.
- Urinary retention is the accumulation of urine in the bladder; more than 500 mL of urine produces a bulge in the central lower abdomen just above the symphysis pubis when the client is in the supine position.
- May be difficult to identify in an obese client.
5. Use a bladder ultrasonic scanner to assess for the amount of urine retained in the bladder after voiding (residual urine); this assessment is more objective than palpation and percussion.
6. Auscultate the abdominal aorta and renal arteries for an adventitious sound of arterial blood flow; presence indicates a vascular problem.
7. Assess perineal skin integrity.
- Assess for presence of a perineal rash with macerated skin (ammonia contact dermatitis), which may extend to the thighs and usually is caused by urinary incontinence.
- Assess for the presence of a perineal red rash with satellite lesions, which may extend to
the thighs and is related to a fungal infection (Candida rash).
8. Assess the vaginal vault for clinical manifestations of atrophic vaginitis (e.g., dry, thin mucosa; tenderness; pallor; easy bleeding).
9. Assess the client’s mental status, mobility, dexterity, and visual acuity to determine ability to self-toilet.
10. Assess for the presence of a urinary diversion.
V. Urinary System Diagnostic Tests and Related Nursing Care
A history and physical may need to be supplemented with data collected via diagnostic tests prescribed by the primary health-care provider. Some tests are essential to arrive at a medical diagnosis (e.g., urine culture and sensitivity, cystoscopy), whereas others are employed to identify specific information about a client’s urinary function (e.g., blood chemistry tests, urodynamic studies). Nurses must understand these tests because some of them are performed by the nurse, some require specific nursing interventions before and after the test, and all of them require client teaching.
A. Urine specimens
1. Commonalities of nursing care when collecting a urine specimen.
- Wash your hands and collect the necessary equipment.
- Explain the procedure to the client.
- Wear clean gloves to prevent exposure to the client’s body fluids.
2. Urinalysis.
- A urinalyisis the physical, chemical, and microscopic examination of urine to aid in the medical diagnosis.
- Macroscopic and microscopic analysis of urine for normal and abnormal constituents (physical and chemical); includes color, turbidity, pH, specific gravity, protein, glucose, ketones, red blood cells, white blood cells, bacteria/yeast, and casts (precipitation of protein substances).
- Specific nursing care.
- Instruct the client to void into a clean bed pan, urinal, or specimen hat positioned under the toilet seat if transferring 30 mL of urine to a traditional clean urine specimen cup.
- Teach to avoid contaminating the specimen with feces, toilet tissue, or menstrual blood; if the client is menstruating, note it on the laboratory slip.
- For infants, wash the genital area, allow the area to dry, and then place a collection device over the infant’s genital area.
- Move urine to a transfer container if a bedpan, urinal, or hat is used to collect urine.
- Use a urine transfer “straw” with adaptor to transfer the specimen to an evacuated urine collection tube.
- Pour 30 mL into a traditional specimen container carefully.
- If a urine collection container with an integrated port in the lid was used to collect the urine, insert a collection tube into the special access port. The closed system automatically transfers the urine to the collection tube via a vacuum.
- Label the container (specimen cup or collection tube) with the client’s name, date, and time of collection according to agency policy and place it in a biohazardous bag to reduce the transmission of infection.
- Assist the client with perineal and hand hygiene.
- Clean or dispose of supplies.
- Remove gloves and then wash hands.
- Document the procedure in the client’s clinical record.
- Send the specimen to the laboratory with the appropriate laboratory slip within 15 minutes; place the specimen in a specimen refrigerator if a delay occurs.
3. Clean-catch (midstream) specimen.
- A clean-catch urine specimen provides a specimen with minimal introduction of microorganisms from the perineal area.
- Specific nursing care.
- Maintain sterility of the urine specimen cup by turning the inside of the lid of the cup toward the ceiling when placing it on a clean surface, avoiding touching the perineum with the cup, and closing the lid without touching the inside of the cup or lid.
- Collect urine or teach the client how to collect the urine.
- For males: Retract the foreskin to expose the urinary meatus if the client is uncircumcised; clean the urinary meatus in a circular motion with three different swabs; have the client begin voiding; after some urine is voided, position the sterile container under the stream and collect the specimen; allow the client to finish voiding; return the foreskin to the expected position if necessary; and close the container without contaminating the inside of the cup or lid.
- For females: Separate the labia minora and cleanse the area from the pubis to the rectum with three different swabs; have the client begin to void while keeping the labia separated; allow urine to flow and then hold the sterile specimen cup under the stream and collect the specimen; remove the container; release the hand from the labia; allow the client to finish voiding; and close the container without contaminating the inside of the cup or lid.
4. Twenty-four-hour urine specimen.
- Measures kidneys’ excretion of substances, such as protein, uric acid, creatinine, selected hormones, urobilinogen, and other substances, that the body does not excrete at an even rate throughout the day.
- Specific nursing care.
- Explain the need to collect all urine for the next 24 hours.
- Post reminders for the client and staff on the bathroom door if permitted by policy.
- Check with the laboratory whether the specimen container has a preservative or needs to be kept in a basin of ice.
- Begin by having the client void, discard this urine, and record the time.
- Collect all voided urine during the next 24 hours.
- Have the client void at the end of the 24 hours and add this urine to the container.
- If the client fails to collect a voiding, have the client empty the bladder and begin the 24 hours again.
5. Culture and sensitivity.
- Identifies the causative microorganism and the most effective antibiotic to eradicate the microorganism; takes 24 to 72 hours for organisms to multiply and be identified.
- Specific nursing care.
- Collect a clean-catch urine specimen or a specimen from a urinary catheter.
- Maintain surgical asepsis to prevent contamination of the specimen.
- Obtain the urine specimen before the client takes a prescribed antibiotic.
6. Dipstick testing of urine.
- Provides a quick, bedside assessment of specific constituents of urine (e.g., pH, specific gravity, protein, glucose, ketones, and occult blood).
- Specific nursing care.
- Ensure that the correct strip is used and that it has not expired.
- Dip the test strip into the urine, tap the strip to dislodge excess urine, and place the strip horizontally across the top of the urine cup to prevent urine from flowing down the strip or collecting at one site on the strip, causing inaccurate results.
- Begin timing according to the manufacturer’s directions and at the correct time; compare the results to the color chart on the dipstick bottle.
- Document the results in the client’s clinical record and report any abnormalities to the primary health-care provider.
7. Collecting a urine specimen from a urinary catheter.
- Specific nursing care when collecting a specimen via a single-lumen catheter.
- Insert a single-lumen urinary catheter into the bladder following all the principles associated with surgical asepsis.
- Collect the specimen and then immediately remove the catheter.
- Specific nursing care when collecting a specimen from an indwelling urinary catheter.
- Ensure that the drainage tube is free from urine and then clamp it below the level of the specimen port on the drainage tubing for 15 to 30 minutes, allowing fresh urine to collect.
- Wash your hands and don clean gloves.
- Clean the specimen port with an alcohol swab.
- Insert the needle of a sterile syringe into the port and aspirate the required amount of urine.
- Transfer the specimen to a sterile specimen cup.
- Discard the needle and syringe into a sharps disposal container.
- Close the lid tightly on the specimen cup without contaminating the inside of the cup or lid. Transfer the urine to a collection tube if it is the protocol of the agency.
- Maintain the closed drainage system; never separate the catheter from the drainage tubing to collect a specimen because it creates a portal of entry for microorganisms, and never collect a specimen from the collection bag because the urine is not fresh.
- Remove the clamp from the drainage tubing.
B. Blood chemistry tests
1. Blood urea nitrogen (BUN).
- Blood urea nitrogen reflects the level of urea nitrogen, a by-product of protein metabolism, in blood.
- Expected level is 10 to 20 mg/dL.
- Increased levels.
- Occur in kidney disease because urea excretion is decreased.
- Can also occur due to digested blood from gastrointestinal (GI) bleeding, dehydration, high-protein diet, steroids, strenuous activity, and nephrotoxic drugs.
- Decreased levels.
- Generally indicate overhydration.
- Can also be caused by severe liver damage, a low-protein diet, malnutrition, phenothiazine medications, and IV glucose without protein intake.
- Specific nursing care.
- Keep the client on nothing-by-mouth (NPO) status for 8 hours.
- Avoid hemolysis of the specimen (e.g., avoid shaking the specimen tube and send the specimen to the lab immediately).
- Identify drugs the client is taking that may increase BUN (e.g., antibiotics, diuretics, antihypertensives, nephrotoxic drugs, sulfonamides, morphine, and salicylates).
2. Creatinine level.
- Creatinine level reflects the level of creatinine, a by-product of muscle catabolism, in blood.
- Expected level is 0.5 to 1.5 mg/dL.
- More than 2.5 mg/dL is indicative of kidney impairment.
- Is more reliable than BUN in determining kidney function because the level is not affected by diet or fluid intake.
- Specific nursing care. (1) Instruct the client to avoid eating red meat the night before the test. (2) Identify drugs that the client is taking that may increase levels (e.g., cefazolin [Ancef], methyldopa [Aldomet], cephalothin [Keflin], gentamicin, ascorbic acid, barbiturates, and lithium).
C. Intravenous pyelogram (IVP)
1. Radiopaque dye injected intravenously concentrates in urine.
2. Facilitates x-ray visualization of kidneys, ureters, and bladder.
3. Is risky when a client has kidney failure because it requires use of a dye that can stress the kidneys.
4. Specific nursing care.
- Obtain an informed consent.
- Explain that the client may experience a warm, flushed sensation or a salty taste when the dye is injected.
- Explain that it takes about 1 hour to complete; x-ray films are taken at various intervals as the dye moves through the urinary system.
- Ensure that an enema or a laxative is taken before the procedure, as prescribed, to ensure that stool and gas do not interfere with the test.
- Explain food and fluid restrictions if prescribed.
- Encourage the client to void before the examination.
- Encourage increased fluid intake after the procedure to facilitate excretion of the contrast/ radioactive substance.
- Monitor I&O after the procedure to assess kidney function.
- Assess for reactions to the contrast media (e.g., rash, nausea, and hives) during and after the test.
D. Ultrasound tests
1. Noninvasive tests using high-frequency sound waves to create an image of the urinary system. Conducted by a certified ultrasound technician.
2. Can identify the amount of urine in the bladder, masses, cysts, edema, and stones.
3. Safe for clients with kidney failure because they do not require dye.
4. Commonalities of nursing care for clients having ultrasound tests.
- Explain the test, including the fact that it will be painless.
- Provide privacy.
- Explain that a conductive gel is applied to the skin and that a transducer is moved smoothly back and forth over the gelled site while a machine visualizes structures of the urinary system.
- Provide hygiene after the test to remove the conductive gel.
5. Bladder ultrasound scan

- Noninvasive test using sound waves to detect the amount of urine in the bladder.
- Provides data for determining the need for catheterization.
- Can be done at the bedside by trained caregivers, including nurses educated in this procedure.
- Specific nursing care.
- Place the client in the supine position.
- Expose only the lower abdomen and suprapubic area.
- Turn the scan device on to female or male; use male if the client had a hysterectomy.
- Use an ultrasound gel pad or 5 mL of conducting gel to improve ultrasound conduction.
- Place the scan head approximately 1.5 inches (4 cm) above the pubic bone midline below the umbilicus (symphysis pubis), aiming the scan head toward the client’s coccyx.
- Press the scan head button, wait until it beeps, and release the button.
- Look for bladder volume to be displayed.
- Repeat the measurement because several measurements ensure accuracy.
- Clean the client’s abdomen and suprapubic area after the procedure to remove conducting gel.
- Clean the scan head with isopropyl alcohol.
- Wash your hands.
- Document the results and client responses in the client’s clinical record.
E. Cystoscopy
Video: Cystoscopy
1. Insertion of a fiberoptic tube through the urethra to directly visualize the inside of the bladder (cystoscopy)to identify stones, lesions, tumors, irritation, or structural problems.
2. Allows specialized instruments to be passed through the tube to take a biopsy or remove small stones or to provide local treatment.
3. Nursing care.
- Obtain a signed consent form.
- Explain that urine may be pink initially after the procedure because of slight bleeding due to irritation of the mucous membranes of the urinary tract.
- Encourage increased fluid intake before and after the procedure.
- Administer antibiotics before and after procedure if prescribed; increasing evidence indicates antibiotics are not necessary for most clients.
- Maintain bed rest initially after the procedure because orthostatic hypotension may occur.
- Assess I&O after the procedure because urinary retention may occur.
- Assess for hematuria, dysuria, bladder spasms, and clinical manifestations of infection after the test. Report these responses to the primary health-care provider.
F. Urodynamic studies
1. Measure stored urine, its flow and elimination in the lower urinary tract, bladder and urethra pressure, and muscle activity.
2. Include the use of uroflowmetry, cystometrograms, and urethra pressure profile measuring devices.
3. Nursing care.
- Encourage the client to drink fluid so that the bladder is full before the test.
- Explain to the client that a catheter will be inserted through the urethra into the bladder as part of the test.
- Encourage the client to drink 8 to 10 glasses of fluid after the test to flush the urinary structures; administer STAT antibiotic if prescribed.
- Teach the client clinical manifestations of UTI and instruct the client to notify the primary health-care provider if any occur.
VI. Nursing Care to Assist Clients With Urinary Elimination
Nursing interventions related to the urinary system involve activities concerning the assessment of a client’s urinary status, collection of specimens for diagnostic tests, promotion of efficient urinary functioning, and the prevention and treatment of urinary problems. Many of these interventions are independent functions of the nurse; however, some require a primary health-care provider’s prescription. Nurses must have a thorough understanding of when and how to implement these interventions.
A. Independent nursing interventions
1. Assess the client’s urinary functioning and the amount and characteristics of urinary output.
2. Encourage the client to follow consistent daily routines.
3. Encourage the client to engage in regular exercise to help maintain pelvic floor and bladder muscle tone.
4. Encourage the client to drink 8 to 10 glasses of fluid daily.
- Provide hourly goals for intake.
- Keep fluids in easy reach.
- Provide fluids that the client prefers.
5. Assist the client with toileting as soon as the need to void is indicated by the client.
6. Provide privacy during toileting.
7. Encourage the client to void (e.g., when the urge to void is felt; on awakening, after meals, and at bedtime; every 2 hours when awake).
8. Encourage the client to completely empty the bladder when voiding to prevent urinary stasis.
9. Assist with positioning.
- Female: Sitting.
- Male: Standing or side lying.
10. Provide a commode at the bedside for clients who are unable to ambulate to a bathroom.
11. Assist bed-bound clients to use a bedpan; remove the bedpan as soon as the client is done voiding; provide perineal care.
12. Promote urination.
- Put the client’s hands in warm water.
- Turn on a sink faucet so that the client can hear the sound of running water.
- Pour warm water over the client’s perineum.
- Place a warm moist wash cloth over the client’s perineum.
- Apply manual pressure over the client’s bladder (Credé maneuver).
13. Teach the client techniques to prevent UTIs.
14. Provide nursing care for clients who are incontinent of urine.
15. Teach the client about prescribed diagnostic tests and the interventions to self-perform in relation to various tests.
B. Dependent nursing interventions
1. Implement care that prepares a client for a test that requires a prescription (e.g., NPO, medications, enema).
2. Obtain urine specimens for prescribed diagnostic tests.
3. Insert and maintain urinary catheters as prescribed.
4. Provide nursing care for clients with a urinary diversion.
5. Administer prescribed kidney-specific anti-infectives, urinary antispasmodics, and estrogen; teach the client information about the medications and self-administration of the medication regimen.
VII. Nursing Care for Clients With Urinary Elimination Problems
Urinary incontinence, UTI, nocturnal enuresis, and urinary retention are common problems related to the urinary system. It is essential that nurses understand the clinical manifestations, precipitating factors, and nursing care associated with each problem. Nursing interventions include activities concerned with promotion of efficient urinary functioning and the prevention and treatment of urinary problems. Many of these interventions are independent functions of the nurse; however, some require a primary health-care provider’s prescription or a standing protocol.
A. Urinary incontinence
1. Overview.
- Urinary incontinence is the inability to control the passage of urine.
- May be acute and reversible (e.g., when due to infection or medication side effect) or chronic and nonreversible (e.g., when due to neurological problems, such as spinal cord injury).
2. Clinical manifestations.
3. Commonalities of nursing care for clients with urinary incontinence.
- Independent nursing care.
- Provide perineal care immediately after voiding or on a regular schedule.
- Encourage the use of/or apply an appropriate incontinence device (e.g., pads, Depends, external condom catheter); avoid the use of the word “diaper.”
- Apply an external condom catheter for a male client.
- Provide perineal care; rinse and dry thoroughly.
- Avoid lubricants or the catheter will slide off.
- Measure the circumference of the penis to ensure correct catheter size.
- Hold the penis and place the condom over and beyond the glans penis; unroll the condom the full length of the penis, leaving 1 to 2 inches between the glans penis and drainage tubing of the catheter.
-
-
- Do not retract the foreskin if the client is uncircumcised.
- Secure the condom: For a condom with internal adhesive, grasp the penis and gently compress so the entire condom comes into contact with the penile shaft; for a condom with an external adhesive strip, wrap the strip in a spiral along the shaft but do not overlap the ends or use surgical tape because these actions can act as a tourniquet.
- Ensure that the condom is not twisted to prevent trauma (e.g., obstruction of urine flow, irritation at meatus, skin breakdown).
- Secure the catheter to the thigh to prevent tissue trauma.
- Encourage necessary lifestyle changes, such as cessation of smoking, weight management, and dietary changes.
- Assess for clinical manifestations of a vaginal infection or UTI, such as hematuria, dysuria, and vaginal irritation.
-
- Dependent nursing care.
- Apply a perineal skin barrier as per agency protocol.
- Administer medications as prescribed.
- Teach the client how to use a prescribed anti-incontinence device (e.g., intravaginal support [pessary], penis clamp, internal urethral meatus plug).
4. Specific nursing care for clients with stress and/or urge incontinence.
- Teach the client to avoid constipation: Increase fluid intake, eat high-fiber foods, and increase activity.
- Teach the client to limit activities that increase intra-abdominal pressure (e.g., high-impact exercises, lifting, bending).
- Encourage the client to perform Kegel exercises to strengthen the pelvic floor.
- Tighten the pelvic muscles as if to stop urination or passing of gas.
- Hold for 5 to 10 seconds and then rest 5 to 10 seconds.
- Repeat two to four times a day with 15 repetitions per session.
- Explain to the client that it may take 6 to 12 months for positive results.
- Teach vaginal weight training to females if prescribed.
- Insert a small cone-shaped weight into the vagina and contract the pelvic floor muscles to keep it in place.
- Keep the cone-shaped weight in the vagina for 15 minutes twice a day.
- Employ a bladder retraining program, particularly for clients with urge incontinence (e.g., using a voiding diary; scheduling regular times for voiding; using distraction and relaxation techniques to relax the detrusor muscle, thereby increasing bladder capacity).
- Administer prescribed medications to relax the detrusor muscle and increase bladder capacity (e.g., anticholinergics, smooth-muscle relaxants, calcium channel blockers, antidepressants) and estrogen for women who have genital atrophy.
5. Specific nursing care for clients with overflow incontinence.
- Identify distension of the urinary bladder: Bladder scan indicates urinary volume; palpation reveals smooth, round, tense mass in suprapubic area.
- Insert a single-lumen or indwelling urinary catheter if prescribed.
6. Specific nursing care for clients with reflex incontinence.
- Precipitate urination: Stroke inner thigh, pull on pubic hair.
- Insert a single-lumen urinary catheter if prescribed.
- Administer prescribed medications to relax the urinary sphincter such as diazepam (Valium).
7. Specific nursing care for clients with functional incontinence.
- Teach the client to schedule routine toileting, especially 15 minutes before the identified pattern of incontinence.
- Teach the client methods to facilitate toileting: Velcro clothing closures, bedside commode or urinal, gait and strength training, raised toilet seat, and bathroom grab bars.
B. Urinary tract infection
1. Overview.
- Urinary tract infection occurs when there is an invasion of the bladder by bacteria, viruses, or fungi; Escherichia coli,which normally resides in the colon, most commonly invades the urinary tract.
- May occur in the urethra (urethritis), bladder (cystitis),ureters, kidneys (pyelonephritis).
2. Clinical manifestations.
- Burning on urination (dysuria).
- Bladder spasms or back pain.
- Frequency.
- Hematuria.
- Chills; fever.
- Pus in the urine (pyuria).
- Foul odor to urine.
- Positive urine culture.
3. Precipitating factors.
- Sexual activity; use of spermicidal contraceptive gel.
- Dryness of the mucosa and decrease in normal flora due to aging.
- Presence of an indwelling urinary catheter.
- Illnesses that affect the kidneys (e.g., diabetes mellitus, renal calculi).
- Conditions that cause urinary stasis (e.g., prostate gland enlargement, hypotonic bladder).
4. Independent nursing care.
- Teach the client clinical manifestations of UTI.
- Provide perineal care immediately after voiding or on a regular schedule.
- Encourage the use of or apply an incontinence device (e.g., pads, Depends, external condom catheter).
- Teach the client preventative measures.
- Void every 2 to 4 hours, not just in response to the urge.
- Avoid food and beverages that can irritate the bladder (e.g., citrus fruits, caffeinated beverages, alcohol, and some spices).
- For women: Wear cotton underwear; void before and after intercourse; avoid bubble and baking soda baths, perineal deodorant sprays, and douches.
- Drink at least 24 oz of cranberry juice daily.
5. Dependent nursing care.
- Collect a urine specimen before initiating antibiotic therapy.
- Apply a topical barrier to maintain skin integrity per agency protocol.
- Administer prescribed medications.
- Antibiotics, such as cephalexin (Keflex), nitrofurantoin (Macrobid), and sulfonamides (e.g., Bactrim, Septra), to eradicate the causative organism.
- Urinary analgesics, such as phenazopyridine, to limit discomfort.
- Anticholinergic drugs, such as oxybutynin (Ditropan, Oxytrol), to inhibit involuntary bladder contractions.
C. Nocturnal enuresis
1. Overview.
- Nocturnal enuresis the involuntary passage of urine when asleep.
- Occurs after voluntary control should have been established.
2. Clinical manifestations.
- Urinating when asleep.
- Person fails to awaken when the bladder empties.
3. Precipitating factors.
- Health problems that interfere with the ability to concentrate urine.
- Health problems associated with excessive urine output (e.g., diabetes mellitus, diabetes insipidus).
- UTIs.
- Trauma or diseases of the spinal cord.
- Structural defects of the urinary tract.
- Misguided attempts at toilet training.
- Emotional stressors (e.g., birth of sibling, illness or death in the family, separation from family).
4. Independent nursing care.
- Include the client in formulating a plan of care; offer hope and encouragement that the plan will work.
- Train the bladder to hold larger amounts of urine when awake (e.g., gradually increase time between voiding).
- Teach family members not to make the client feel guilty or ashamed.
- Encourage the client to avoid fluid intake after the evening meal.
- Encourage the client to empty the bladder just before going to bed.
5. Dependent nursing care.
- Administer prescribed medications.
- Tricyclic antidepressants, such as imipramine (Tofranil); administer at bedtime; ensure monthly blood tests to assess for granulocytosis; question the prescription for a child younger than age 6 years; must be gradually reduced over 6 days to prevent withdrawal.
- Anticholinergics, such as oxybutynin (Ditropan); teach parents to assess for clinical manifestations of urinary retention.
- Teach the client to use a bed alarm, which awakens the client when voiding, only if prescribed by a primary health-care provider trained in the treatment of enuresis; its use is controversial
D. Urinary retention
1. Overview.
- Urinary retention is the accumulation of urine in the bladder due to an inability to empty the bladder completely.
- Excessive distention of the urinary bladder impairs contractility of the detrusor muscle, further impairing urination.
2. Clinical manifestations.
- Suprapubic distention.
- Reported feeling of bladder fullness and discomfort; inability to void despite presence of urge.
- Overflow incontinence exhibited as frequent urination of small amounts of urine.
3. Precipitating factors.
- Factors that cause inflammation and swelling of the genitourinary tract (e.g., infection, childbirth, and pelvic surgery).
- Neurological problems that affect the brain, spinal cord, or peripheral nerves (e.g., brain attack, tumors, and blunt trauma to neuro logical tissue).
- Infection (e.g., genital herpes).
- Obstructions (e.g., enlarged prostate, strictures, tumor, urinary calculi, and fecal impaction).
- Medications (e.g., antihistamines, tricyclic antidepressants, beta-adrenergic blockers, monoamine oxidase inhibitors, antispasmodics, anti-parkinsonism medications, opioids, and anesthetic agents).
4. Independent nursing care.
- Monitor I&O.
- Palpate the suprapubic area for bladder distention.
- Encourage the client to use a position that facilitates voiding by the use of gravity.
- Provide privacy when toileting.
- Use techniques to encourage voiding (e.g., warm washcloth on perineum, placing hands in warm water, running a faucet).
5. Dependent nursing care.
- Assist the client with a warm-water bath that exposes just the perineal area to the water (sitz bath).
- Measure postvoiding residual (e.g., catheterization with a single-lumen tube, bladder ultrasound).
- Insert a single-lumen catheter or indwelling urinary catheter as prescribed.
- Provide preoperative and postoperative care for a client having surgery to remove an obstruction, such as prostate surgery.
- Teach intermittent self-catheterization to drain the bladder for clients with spinal cord injuries or neurological disorders.
VIII. Urinary Catheters
A urinary catheter may be inserted into the urinary bladder via the urethra to collect a specimen, empty the urinary bladder and then be removed, or remain in place to mitigate a problem. The insertion of a urinary catheter is a dependent function of the nurse and requires a prescription. There are various types of urinary catheters, each with its own distinct purpose. The nurse must know the principles associated with urinary catheter insertion, nursing care common to all types of urinary catheters, and nursing care specific to each type of catheter to ensure that the client’s urinary elimination needs are met based on established standards of nursing practice.
A. Purpose
- Obtain a sterile specimen.
- Maintain an empty bladder during diagnostic tests and during or after surgical procedures.
- Treat or prevent urinary retention.
- Measure the volume of residual urine.
B. Types
1. Single-lumen (straight) catheter.
- Single-lumen tube inserted through urethra; used to obtain a sterile urine specimen, to measure residual urine after voiding, or for the immediate relief of urinary retention.
- Immediately removed when bladder is emptied of urine.
2. Indwelling catheter (retention catheter).
- Double-lumen tube inserted through urethra; used for continuous bladder drainage.
- One lumen to inflate the balloon to keep the tube in place and a second lumen to drain urine.
3. Triple-lumen catheter.
- Triple-lumen tube inserted through urethra or suprapubic area; used for continuous bladder irrigation.
- One lumen to inflate the balloon, second lumen to continuously instill a GU irrigant, and third lumen to drain urine and irrigant into a collection container.
4. Suprapubic catheter.
- Double-lumen tube inserted through suprapubic area; used for continuous bladder drainage when the urethral route is contraindicated.
- One lumen to inflate the balloon to keep the tube in place and a second lumen to drain urine.
C. Insertion of a urinary catheter
1. Explain what is going to be done and why, provide privacy, and wash your hands.
2. Position the client in the supine position, and drape the client, exposing only the perineal area.
- Women: Flex the knees, and allow the thighs to externally rotate; Sims’ position with the upper leg flexed is also acceptable.
- Men: Slightly separate the legs with the knees and hips extended.
3. Don clean gloves, wash the perineal area, remove your gloves, and wash your hands.
4. Arrange the work area.
- Open a sterile catheter kit on a clean bedside table without contaminating the inside.
- Arrange a trash receptacle impervious to liquid in easy reach.
5. Don sterile gloves and maintain their sterility throughout the procedure.
6. Place the first sterile drape in position without contaminating the drape.
- Women: Under the perineal area.
- Men: Across the thighs.
7. Position the second sterile drape with the opening (fenestrated drape) arranged so that the urinary meatus is visible.
- Women: Over the perineum with the hole over the labia.
- Men: Over the thighs with the hole over the penis.
8. Organize the sterile supplies in the catheter kit.
- Pour the antiseptic solution over the cotton balls.
- Arrange the forceps near the cotton balls.
- Squeeze sterile lubricant into the kit tray.
- Connect the syringe to the catheter port.
- Roll the catheter tip in the lubricant (a length of 2 inches for women and 8 inches for men).
9. Position the catheter kit on the sterile field.
- Women: Between the client’s legs.
- Men: On top of the thighs or between the client’s legs.
10. Place the collection bag on the field or nearby if it is pre-attached to the catheter and tubing.
11. Cleanse the urinary meatus.
- Women: With one hand, spread and gently pull the labia majora and minora upward, exposing the urinary meatus, and hold this position throughout the procedure; with the other hand, hold an antiseptic-soaked cotton ball with the forceps and wipe from the pubis to the rectum along the far labia and then discard the cotton ball in the trash receptacle; repeat this along the near labia and then down the middle using a new cotton ball each
- time.
- Men: Reach through the fenestrated drape and grasp the penis (retract the foreskin if the client is uncircumcised) and hold this position throughout the procedure; with the other hand, hold an antiseptic-soaked cotton ball with the forceps and wipe in a circular motion from the center of the urinary meatus outward and down the penis and then discard the cotton ball in the trash receptacle; repeat this two more times using a new cotton ball each time.
12.Women: Insert the lubricated end of the catheter 2 to 3 inches into the urinary meatus until urine begins to flow into the tubing and then advance it 1 more inch (this ensures that the catheter has completely passed through the urethra); encourage the client to take deep breaths to facilitate relaxation; if the catheter touches unsterile linen or the labia or vagina, it is no longer sterile and a new sterile catheter must be used.
- Men: Insert the lubricated end of the catheter 7 to 9 inches into the urinary meatus until urine begins to flow and then advance 1 more inch to ensure that the catheter has completely passed through the urethra; do not force catheter insertion if resistance is felt; lower the penis when the bladder is empty; replace the foreskin if the client is uncircumcised.
13. Hold the catheter in place and, with the other hand, inflate the balloon using the attached saline-filled syringe; if the client complains of discomfort, deflate the balloon, advance the catheter 1 inch, and reinflate the balloon because the catheter may be in the urethra.
14. Discard used supplies, remove your gloves, and wash your hands.
15. Hang the urine collection bag on the bed frame rather than on a side rail to prevent trauma to the urinary meatus and bladder when the side rail is moved.
- Always hang a urine collection bag below the level of the bladder to promote urine flow by gravity and prevent back flow of urine into the bladder.
- Keep the urine collection bag off the floor and coil the loops of the tubing on the bed to avoid dependent loops.
16. Secure the catheter to the client’s thigh for females or abdomen for males (e.g., using catheter strap, tape) to prevent tension on the tubing and trauma to the bladder and urinary meatus.
17. Don clean gloves, cleanse the perineal area, and remove your gloves.
18. Return the client to a comfortable position and wash your hands.
19. Document the amount and characteristics of urine and the client’s response to the procedure.
D. Nursing care for clients with an indwelling urinary catheter
1. Perform routine assessments.
- Monitor I&O.
- Monitor urine characteristics.
- Assess the perineal area for clinical manifestations of an infection of skin and mucous membranes.
- Assess for clinical manifestations of a UTI.
2. Provide care to prevent a UTI.
- Keep the collection bag below the level of the bladder by attaching it to the bed frame and coiling the tubing on the bed to prevent dependent loops.
- Maintain a closed system to prevent the introduction of pathogens by maintaining the integrity of all connections; if the tubing becomes disconnected, wipe both ends of the tubing with an antiseptic solution before reconnecting them.
- Secure the tubing to the client’s anterior thigh for females and lower abdomen in males; this limits tension on tubing and helps to prevent lying on the tubing.
- Wash the perineal area and around and down the catheter with mild soap and water and rinse and dry thoroughly every 8 hours; avoid using powders and lotions after perineal care because these products provide a medium for the growth of microorganisms.
- Encourage ambulation and the upright position to facilitate bladder emptying if permitted.
- Encourage the intake of 3 L of fluid daily, if permitted, to help flush the urinary tract.
- Encourage the intake of foods that increase urine acidity (e.g., cranberry juice, eggs, meat, poultry, whole grains, plums, prunes, and tomatoes); acidic urine discourages the growth of microorganisms.
- Discourage the intake of foods that increase urine alkalinity (e.g., most fruits, vegetables, legumes, milk, and milk products); alkaline urine favors the growth of microorganisms.
- Maintain aseptic technique when emptying the collection bag (e.g., keep the drainage bag off the floor; ensure the spout does not touch the collection graduate or floor).
- Teach the client the importance of meticulous perineal care after a bowel movement.
- Administer a prescribed oral or intravenous antibiotic and a prescribed topical antibiotic or antifungal ointment to the perineal area.
3. Specific nursing care to prevent obstruction of the catheter.
- Ensure the catheter has no mechanical obstructions (e.g., kinks in the tubing, client lying on the tubing).
- Monitor the patency of the tubing every 2 hours, especially if sediment or hematuria is present.
- Ensure that if a clamp is used during a procedure that it is removed promptly after the procedure (e.g., obtaining a urine specimen, instilling a medication into the bladder for a prescribed time frame).
- Instill or irrigate the catheter with sterile normal saline solution as prescribed, especially if the client’s urine has blood clots or large amounts of sediment.
- Change the catheter if drainage is impaired.
E. Removal of a urinary catheter
- Prepare client for removal of the catheter if prescribed: Clamp the drainage tubing distal to the French catheter as specified (e.g., clamp for 2 hours and release for 15 minutes three times a day); this increases bladder tone in preparation for discontinuation of the urinary catheter.
- Use a needleless syringe to remove the fluid in the balloon before removal of the urinary catheter; never use scissors to cut a urinary catheter to drain the balloon because it can compress the lumen preventing removal of the fluid.
Because of a disease process or injury to the urethra, bladder, or ureter, a client may require the creation of a urinary diversion to permit evacuation of urine. An ileal conduit, Kock pouch, nephrostomy tube, suprapubic tube, and ureterostomy tube are types of urinary diversions created for the elimination of urine. To best meet clients’ urinary elimination needs, the nurse must understand each type of diversion, including the way in which it is formed and the way in which it works; the general physical and psychological nursing care of a client with a urinary diversion; and the specific nursing care related to each type of urinary diversion.
A. Types
1.An ileal conduit is when a segment of the ileum is removed and used as a pouch reservoir.
- One end is brought through the abdominal wall to form a stoma. c. Ureters are implanted into the pouch.
- Urine drains continuously.
2. A Kock pouch is formed when a portion of the ileum is used to form a pouch reservoir, which is connected to the skin.
- Ureters empty into the pouch.
- A nipple valve is created surgically and the pouch is emptied by inserting a clean catheter every few hours.
- A small dressing is worn over the nipple stoma between emptying.
- A nephrostomy tube is a tube placed into the pelvis of a kidney to drain urine into a collection container.
- Prevents accumulation of urine and stretching of the renal pelvis (hydronephrosis)due to an obstructed ureter.
4. Suprapubic tube.
- A suprapubic tube is a catheter that is surgically inserted through a small incision above the symphysis pubis to drain urine into a collection container.
- It diverts urine when flow of urine through the urethra is impaired.
- It may be temporary or permanent.
B. Nursing care for clients with a urinary diversion
1. Monitor I&O.
2. Assess site for clinical manifestations of inflammation or infection.
3. Provide emotional support and teach self-care.
4. Keep the skin around the site clean and dry; apply a moisture-proof skin barrier as prescribed to reduce risk of maceration of skin.
5. Apply a prescribed topical antibiotic (e.g., bacitracin) or antifungal (e.g., nystatin) ointment on the skin around the tube entry site.
6. Secure the tubing to the body (e.g., abdomen or flank area) depending on the entry site to reduce tension on the tube.
7. Keep the tubing and collection bag(s) dependent to the site being drained.
8. Empty smaller urine collection devices (e.g., leg bag) frequently; leg bag is used under clothing during the day to facilitate ambulation; attach the tubing to a larger collection device when the client is in bed or at night.
9. Suprapubic tube: In preparation for removal of a temporary tube, clamp the catheter for 3- to 4hour periods during the day as prescribed to assess whether the client is voiding a satisfactory volume through the urethra; residual is measured to determine what is satisfactory.
X. Bladder Irrigations
Instillation of a solution into the urinary bladder may be prescribed to flush the bladder, instill medication into the bladder, or maintain patency of a urinary catheter. Instillations may be intermittent or continuous. The nurse must know the principles of and implement actions related to nursing care associated with both intermittent and continuous bladder irrigations to best meet clients’ urinary elimination needs.
A. Types
- An intermittent bladder irrigationis used to instill medication.
- Used to flush the bladder or to restore catheter patency.
2. Continuous bladder irrigation.
- A continuous bladder irrigation is the constant instillation of an irrigant into the bladder via a three-lumen urinary catheter to maintain catheter patency when hematuria, clots, or debris are anticipated, generally after surgery (e.g., resection of the prostate).
- Requires a triple-lumen catheter: One to inflate the balloon to hold the catheter in the bladder, the second to continuously instill the genitourinary (GU) irrigant, and the third to drain urine and irrigant to a collection device.
B. Nursing care for clients receiving a bladder irrigation
1. Commonalities of nursing care when implementing a bladder irrigation.
- Provide for privacy.
- Assess the client’s comfort, including the presence of painful bladder spasms.
- Assess the urinary catheter often for tube patency.
- Calculate urine output by deducting the volume of irrigant from the total output.
- Document the nursing care provided and client responses in the clinical record.
2. Specific nursing care for clients with a prescription for intermittent bladder irrigation.
- Wash hands and then don clean gloves.
- Cleanse the catheter port with an alcohol swab.
- Compress the drainage tube with the fingers of one hand; this permits the irrigant to flow into the bladder rather than down the tube into the collection bag.
- Instill the irrigant into the port slowly to facilitate the flow of the irrigant into the bladder and limit trauma to the mucous membranes of the urinary tract.
- Allow the solution to return via gravity.
3. Specific nursing care for clients with a prescription for continuous bladder irrigation.
- Connect a 3-L bag of the prescribed solution to the input port of the three-way catheter.
- Adjust the flow rate as prescribed; a specific rate may be prescribed (e.g., 40 to 60 drops per minute) or the rate may be left to the discretion of the nurse to keep output pink and clot free.
- Assess output every 15 minutes to ensure patency of the tubing; if the tubing becomes occluded, bladder distention and fluid backup can cause distention of the pelvis of the kidney and impede kidney function.
- Ensure that the 3-L bag of irrigant is replaced when the previous bag is low on fluid so it does not run out because the flow must be uninterrupted to ensure catheter patency.
XI. Medications That Affect the Urinary System
When a person is diagnosed with a urinary system problem, the primary health-care provider can prescribe medication, such as kidney-specific anti-infectives to treat a UTI; urinary antispasmodics to reduce bladder spasms, increase bladder capacity and decrease incontinence; or estrogen to decrease vaginal and vulvar itching, inflammation, and dryness, which impact the urinary system. Nurses should know the mechanisms of action, therapeutic and nontherapeutic effects, and nursing care related to the common medications prescribed to treat urinary system problems.






